In a stunningly short period of time, the delta variant has changed the course of the COVID-19 pandemic by evolving to become more transmissible than previous versions of the virus.
Compared to the alpha variant, which is estimated to be 50% more transmissible than the original virus strain identified in Wuhan, China, scientists believe the delta variant, now dominant worldwide, is 40% to 60% more transmissible than alpha.
But how exactly did the delta variant evolve into the highly infectious strain that the world is now struggling to contain? Scientists have a few theories. 
“This is a new virus for humans,” explained Adolfo Garcia-Sastre, director of the Global Health and Emerging Pathogens Institute of Icahn School of Medicine at Mount Sinai. “You can think about like a baby. The virus came to humans for the first time. He has not learned still everything.”
The so-called variants of concern — alpha, beta, gamma and delta — show the virus is evolving. “What we are seeing is that there are mutations that are being selected that make the virus even better at transmission,” Garcia-Sastre said. For now, scientists don’t know whether the delta variant, the most transmissible of the four, has reached its full potential for transmissibility. But the more the variant circulates, the more chances it has to evolve and reach full potential to infect humans at maximum scale.
“That’s what makes a winner if you’re a virus — more replication,” he added.
How viruses evolve to be more transmissible
“Every time the virus replicates, or makes a copy of itself, it tries to make a copy that’s identical,” Garcia-Sastre said. But like human cell replication, which can sometimes result in cells with new mutations, viruses make mistakes when they copy themselves. In most cases, those mistakes make the virus weaker. But if a single mutation makes the virus stronger and also manages to infect a new host, “it will start to propagate and start to dominate,” he said. While stronger mutations are the exception to the rule, widespread transmission of the virus means more chances for mutations that could include less common, but stronger variants.
In general, there are a few pathways by which this could happen. High community transmission, as was seen in the United Kingdom and India before the alpha and delta variants were detected there, is one pathway. Another is in people with so-called chronic infections, meaning they are infectious for longer than the typical duration of COVID-19 (not to be confused with long-haul cases), which could occur if someone has a weakened immune system or is taking immunosuppressant drugs.
“Some individuals have a persistent or a prolonged or a chronic infection. Then you have accelerated evolution inside that individual,” said Dr. Richard Lessells, an infectious disease expert at Kwazulu-Natal Research Innovation and Sequencing Platform in Durban, South Africa, where he researches beta, the virus variant first identified in the country.
“If that virus is then transmitted and has some evolutionary advantage in the population, it can spread from there,” Lessells said.
Nevan Krogan, a molecular biologist at the University of California, San Francisco, has collaborated on papers with Garcia-Sastre during the pandemic. “It’s like the mother of all selections in the world. It’s the biggest experiment that’s ever happened,” Krogan said. “We’re forcing the virus to mutate, which it loves to do.” 
In addition to mutations, there is another way that viruses can acquire new changes that may make them more transmissible, according to Garcia-Sastre, although it’s a pathway that’s difficult to study and not well understood. Viral recombination happens when two different parent strains of the virus enter the same cell. They then can combine and make new mixtures when they replicate.
“Someone can get, for example, an alpha and a beta together,” Garcia-Sastre explained. That could explain why the delta variant has 20 mutations, a high number for a virus that has not evolved very quickly.
Still, Garcia-Sastre cautioned of the recombination theory — “it is very difficult to prove.”
While the vaccines are holding up well against the variants in terms of protecting against hospitalization and death, the delta variant is a bit more likely to infect fully vaccinated people — so-called breakthrough cases — than past variants.
“It shows the possible beginning of a trajectory and that’s what worries me,” Aris Katzourakis, an evolutionary biologist at the University of Oxford, told Science magazine in August.
Changes to the virus’s spike protein could make it more transmissible
All four variants of concern have mutations in the virus’s spike protein, the protein that protrudes from the surface and makes it look like it’s wearing a crown.
“The thing that is happening with all of these variants is that they bind better to the receptor,” Garcia-Sastre said. “It finds the cells faster because it binds better to the receptor. If the virus has acquired the ability to bind better, then it has a better chance to start infections.”
While alpha, beta, gamma and delta all have mutations on their spike proteins, they are all different mutations, Garcia-Sastre explained. “That’s what’s interesting. They gain a better ability to process the spike and then a better ability to enter and replicate.”
Beyond spike
“Everyone is focused on spike. Yes, spike is playing a role, no question about it, but there are other mutations that could be equally as important as spike,” said Krogan.
Krogan’s research, which has not yet been published in a scientific journal, suggests that once the alpha variant gets inside a cell, it suppresses the immune response compared to other variants. A suppressed immune response allows the virus to replicate more, resulting in increased transmissibility and ultimately increased mortality, he explained. It could also explain why the alpha variant spreads so rapidly. Now Krogan’s team is doing tests on the delta variant to see if it has similar immune response suppression causing it to be even more transmissible than the alpha variant. “We are investigating if a similar mechanism exists with delta and other variants of concern.” 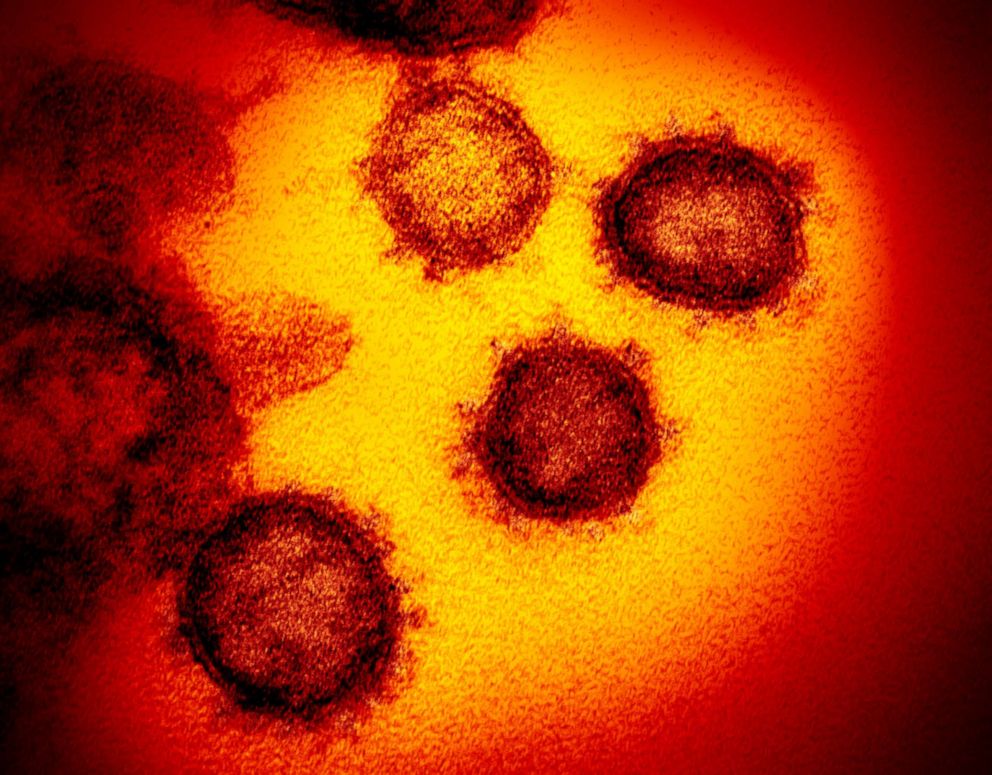
Importantly, as far as scientists can tell, the alpha variant did not evolve into the delta variant. Instead, the two variants developed independently of one another in countries where high community transmission was occurring.
“The alpha variant came from England and the delta variant came from India, it just kind of got to the same place,” Krogan said. “Different mutations could have the same results.”
A glimmer of hope
As vaccinations ramp up in wealthier and well-connected countries, it puts selection pressure on the virus to mutate so it’s able to continue to infect hosts. The only way out is to vaccinate faster or adapt vaccinations to beat out newer versions of the virus as they crop up.
“We’re in this battle with the virus,” Krogan said. “Are we going to use the tools we have right now? Or will those tools become obsolete very quickly?”
Garcia-Sastre struck a more optimistic note on the role of vaccines.
“If you can bring this virus from killing 5 million per year to 500,000 per year, this virus will have the same consequences as an influenza,” Garcia-Sastre said of the power of vaccinations. “If we can reduce the mortality of this virus 10 times by vaccination, the problem is still is there, but now it’s a different problem.”
While having dueling infectious disease threats of the flu and COVID-19 each year would certainly burden the health care system, it would be a significant improvement over the overwhelming crisis that many countries have faced over the past 18 months. “We are not going to be completely able to prevent death — that’s clear — but if we can reduce it at least 20 times, then I think we can say that the pandemic is over,” Garcia-Sastre said.
In his mind, the goal was never getting to COVID zero. “It was quite clear for me that it was going to be very difficult to eradicate this virus,” he said. “But we can make it manageable. Then it will be a nuisance. It’s unfortunate for the people who get severe disease — the same thing as with flu — but at least it is not impacting all the sectors of the society like it is right now.”